The specter of COVID has haunted the globe for four years now—the disease has killed at least seven million people worldwide. Yet the pandemic’s long-term effects are still hazy—because when it comes to a novel virus such as SARS-CoV-2, which causes COVID, scientists still have a lot to learn.
What we do know is that COVID is here to stay—and that catching it doesn’t give people permanent immunity. Four years into the pandemic, researchers and clinicians know that people are racking up multiple infections, but the long-term consequences of repeatedly getting the virus aren’t yet clear. Fortunately, both individuals and governments have strategies to avoid some infections—if they use them.
“However you slice it, whatever long-term health effect you look at, the risk [from reinfection] is not zero,” says Ziyad Al-Aly, a clinical epidemiologist at Washington University in St. Louis. “The truth is that, yes, we’re sick and tired of the virus, we’re sick and tired of the pandemic—but it’s still here. It’s still hurting people.”
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
In the U.S. alone, more than 1.1 million people have died of COVID since the pandemic began, according to the Centers for Disease Control and Prevention. The agency is no longer tracking infections at the community level, but in mid-January it reported that nearly four percent of deaths nationwide were caused by COVID.
And while the winter wave of infections appears to be waning, the world missed its chance to make COVID disappear. “This ugly guest isn’t going to leave us any time soon,” Al-Aly says. “It’s going to be here probably for decades.”
Early on in the pandemic, scientists hoped that COVID would be the sort of disease for which vaccination or infection creates immunity that lasts for years or a lifetime. But the SARS-CoV-2 virus had other plans. Vaccination and, to a lesser degree, infection make you less vulnerable to catching the virus and having a severe case, but that protection wanes over time.
“One infection does protect you against future infections” but not completely, says Jamie Rylance, a physician on the World Health Organization’s clinical management team. The SARS-CoV-2 virus mutates rapidly, so a person’s immune system can’t necessarily fully fight off a new infection, even if it’s been primed by a recent bout with a different strain. The same holds true for vaccinations: although initial shots and boosters help a person’s immune system respond more effectively to an infection and reduce the odds of a serious COVID case, current COVID vaccines can’t prevent infection completely.
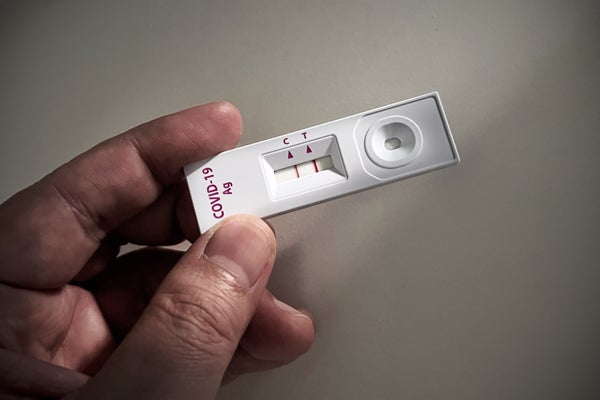
Complicating things further, COVID often triggers asymptomatic infections, which helped the virus continue to spread early in the pandemic even in places where governments established relatively strict containment protocols. And four years into the pandemic, many people are testing for COVID less often and tests miss many asymptomatic cases, making them even harder to identify. So people have likely been infected more times than they know.
“We don’t know how often we’re getting reinfected because we have some protection from vaccination or even past infection,” says Maria Van Kerkhove, interim director of the WHO’s department of Epidemic and Pandemic Preparedness and Prevention. She doesn’t think that’s something to be complacent about, however. “We know that when the virus enters our body, it affects multiple organ systems,” she says.
The combination of evidence on COVID and the long-term impacts of other viruses paints a grim picture of what it might mean to experience regular COVID infections.
“Every time you get infected [with COVID], it does harm to the body in some way,” says Avindra Nath, a neurologist at the National Institutes of Health who has led research on long COVID and other postviral conditions. For example, a pulmonary infection can leave scars in the lungs or trigger blood clots. COVID may also interfere with the immune system itself, he says. Nath notes that the protective sheaths of many viruses include regions that can interfere with the immune system. Separately, one study that followed up with participants after a flu infection found that in about 30 percent of people, the immune system remained somewhat impaired two months later.
And because COVID is still relatively new, scientists realistically have no idea what happens 10, 20 or even 30 years after an infection, much less multiple bouts. “What we need to be able to track is the complications of pulmonary function [and] cardiac function five years from now, 10 years from now,” Van Kerkhove says.
Frustratingly, we may never have a clear sense of the damage COVID reinfections are causing, says Sunil Ahuja, an infectious disease specialist at University of Texas Health Science Center at San Antonio. “To ascribe cause and effect is very challenging,” he says of potential long-term consequences of repeated bouts with COVID. During the span of time between infections, “they’ve also had many other things happen to them, too.”
Some viruses can hide out in the body and emerge decades after the initial infection to cause new problems. The virus that causes chicken pox, for example, can trigger shingles many years later. And scientists have recently learned that infection with the common Epstein-Barr virus seriously increases the risk of a person developing the autoimmune disorder multiple sclerosis. “I don’t think we’ve seen the end of this movie yet,” Al-Aly says of SARS-CoV-2’s long-term impacts.
Moreover, COVID has already shown its potential to cause lasting harm in the form of long COVID, which can include debilitating fatigue, breathing problems, difficulty thinking, digestive issues and a wide variety of other symptoms. As of mid-2023 long COVID impacted 11 percent of Americans reporting a previous infection—a notable decline from the previous year. Scientists are still working to determine what triggers long COVID, but it’s clear that people can develop the condition after several infections, not just their first encounter with COVID.
“Each time that you have COVID, you have a chance of having post-COVID condition afterwards,” Rylance says, though he adds that “it’s still fairly unpredictable at an individual level.”
While scientists desperately want more data to better understand the ways COVID could shape a person’s health for years to come, the hints available now are worrying, experts say. “There’s a major concern here that people who are getting repeated infections [could] have long-term consequences,” Nath says. “And the data that is coming out suggests that possibility.”
Although COVID is now endemic and widely circulating, people and societies can both work to minimize the odds of infection, Van Kerkhove and Al-Aly say. For individuals, getting vaccinated and masking in public and crowded spaces remain the most effective strategies for avoiding COVID or reducing the severity of an infection. Unfortunately, just one in five adults in the U.S. had gotten the updated 2023-2024 COVID vaccine as of mid-January, according to the CDC—even though initial analysis of the vaccines shows that they are about 50 percent effective against infections, including by the latest subvariant, known as JN.1. Testing for COVID when feeling unwell and using antiviral medications such as Paxlovid also remain vital tools for reducing disease risk.
WHO’s Van Kerkhove says that government action is key, including ensuring that masks, vaccines, tests and treatments are available and affordable. But she also called on governments to take bolder steps such as strengthening ventilation requirements in buildings and supporting the development of better vaccines, including an oral or nasal vaccine that could more effectively prevent against COVID in the respiratory tract, where the virus enters a person’s body. In addition, Al-Aly says, we need a longer-lasting vaccine that would offer meaningful protection for several years, so people would not need to get vaccinated every year.
“It’s not beyond the might of U.S. medicine to really develop the technology and to deliver those solutions,” Al-Aly says of such next-generation vaccines. He says the investment is particularly important now that we understand that COVID is not a problem we will dispense with quickly—and now that concerns are mounting about the damage of repeated infections.
“Those are going to be the long-term, sustainable solutions,” Al-Aly says. “It isn’t sustainable to ask people to mask for the next 100 years.”