In June 2022 I sat shaking my head as I heard from senior U.S. government officials that mpox (then monkeypox) was under control. At the time, my dear friend back home in New York, to whom I’d spoken on the phone, had mpox.
I knew the government officials were wrong. If they weren’t outright lying, they were at least using a lack of available testing to minimize a growing epidemic. My friend described the crushing pain of the lesions inside his rectum as making every waking moment feel like he was “shitting glass.” The pain and fever made sleep near impossible.
Now new research published last month confirms what we knew then: a lack of testing led to a significant underestimation of the global mpox spread prior to July 2022. We should have had this genetic information about the epidemic then, and we should have it sooner in the next outbreak, to save lives and prevent unnecessary suffering.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
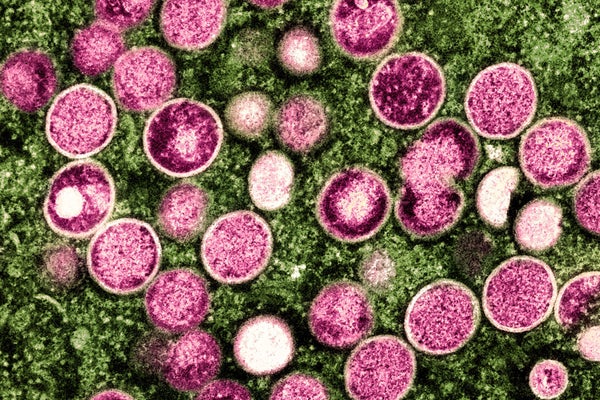
Mpox is a skin infection caused by a virus endemic to countries in West and Central Africa. For decades mpox epidemics—from the Democratic Republic of the Congo (DRC) to Nigeria—have grown in size and frequency. In 2022, mpox went global, with case numbers now nearing 100,000 worldwide. This global outbreak spread mostly via sex and mostly within queer sexual networks.
As an activist and molecular biologist, I was a small part of a large coalition that debunked the CDC’s early numbers on mpox testing and called for their overhaul. The CDC and other government agencies accurately reported that the approved laboratories could run more than 8,000 mpox PCR tests a week. We found, however, that these tests were spread around in states with very few cases, and that labs in cities with large queer populations such as New York City and San Francisco had a capacity of as few as 20 tests a day. By mid-July 2022, when commercial labs began testing, New York City alone reported more than 500 positive mpox tests a week.
A phylogenetics analysis recently published in the journal Cell traced the mpox epidemic through 2022, confirming its early, undetected spread. A phylogeny is akin to a family tree, linking species or individuals by their last common ancestor: humans and chimps, for example, diverged some 12 million years ago. Phylogenies can also trace more recent, and quite rapid, events, such as viral evolution.
Molecular phylogenies begin with sequences of DNA or RNA. DNA contains four “letters” of information: A, C, G and T. Mutations are changes in this code. Under most conditions, biologists have shown that mutations occur at a regular rate, acting as a “molecular clock.” More mutations imply a greater evolutionary distance between viruses. Mutations act like markers as well, where a change from a C to a T may distinguish all the offspring of one particular virus as it moves through a population.
The report’s lead author, virologist Miguel Paredes, told me that “even knowing the existence of a virus circulating in the community a couple of weeks before [testing availability] could actually have a lot of benefit” in terms of curbing the total number of mpox cases in the U.S.
In June 2022, in New York, my friend knew he likely had mpox. He was turned away by his primary care doctor, who tested him for bacterial STIs (he was negative). At the ER, while my friend was in immense pain, a doctor suggested rectal cancer and told him to see a specialist the next week (he did not have rectal cancer). More than a week later, when the city health department finally stepped in, a PCR test confirmed what we all knew: he was infected with mpox.
If the phylogenetic analysis had been available in real time, perhaps public health officials would have acted more quickly, as they did in 2020 when University of Washington researchers alerted local officials to community spread of COVID in the region.
Regardless, early in the mpox outbreak, epidemiology alone offered enough evidence that year to ramp up testing, vaccination and community education. I wonder how many cases could have been prevented—and especially how many U.S.-based mpox deaths, about 90 percent of which were in Black queer people with untreated HIV infections.
While mpox has receded globally, in the DRC an even more deadly strain of the virus is currently spreading unchecked and killing hundreds of people—exceeding the entire global fatality count in 2022. In the DRC, mpox spreads both by close contact, particularly in households, and sexual contact. A majority of diagnosed cases are in children. We have little viral sequence information—and so no ability to build phylogenies—in the current outbreak.
David O’Conner, a virologist at the University of Wisconsin–Madison, told me that COVID initially increased the collaborations between researchers and public health officials. He worries that in our supposedly post-COVID world, we’re returning to a baseline with public health and academics working with “less overlap than during the early [SARS-CoV-2] pandemic.”
Phylogenetics could easily distinguish between the mpox strains that have spread globally since 2022 and those now causing the deadly outbreak in the DRC. A week of data reported by the CDC in late February 2024 included 18 cases of mpox—none of them including information about which strain they were from. Los Angeles County is sequencing positive mpox cases and depositing the data with researchers within weeks. The LA county sequences allow a real-time analysis similar to the research reported in Cell even for cases in 2024, but data are lacking for similar analyses where I live in New York City. Phylogenetics is limited by the amount, timing and location of sequencing, and information coming from only a few well-resourced U.S.-based institutions is inherently biased and unrepresentative.
Real-time genomic analysis in the U.S. could not only estimate the size of ongoing mpox clusters (especially because there may be asymptomatic cases) but could also determine how many cases are the results of local spread versus travel. In the DRC, these types of analyses could similarly estimate the size of the current epidemic and determine the proportion of infections resulting from human-to-human contact versus spillovers from small rodents, the suspected animal reservoir.
Only two years after the global spread of mpox, we are already repeating the mistakes of the past. While the CDC compiles week-by-week data on which SARS-CoV-2 variant is most common in the U.S., these lessons have not been applied to other infectious diseases. There is no public-facing data site on mpox evolution or sequencing.
Paredes puts it bluntly: “Not having surveillance” he says of mpox testing and sequencing, including in Africa, “is really ignoring a lot of preventable suffering and death.” He worries that, given waning vaccine immunity, mpox may return to global spread.
The world’s response to the current epidemic in the DRC has largely been apathy and silence. The incredible insight of the phylogenetic analysis Paredes and his team reported is still only available in an epidemic’s rear-view mirror. According to a recent report, 218 children under 15 died of mpox in the DRC in the first two months of 2024 alone. In Los Angeles, all positive mpox tests are sequenced in full. In the DRC, PCR tests aren’t even used to confirm mpox once a patient has died.
This is an opinion and analysis article, and the views expressed by the author or authors are not necessarily those of Scientific American.