Corlee Morris has dieted throughout her adult life.
After her weight began climbing in high school, she spent years losing 50 or 100 pounds then gaining it back. Morris, 78, was at her heaviest in her mid-40s, standing 5 feet 10½ inches and weighing 310 pounds. The Pittsburgh resident has had diabetes for more than 40 years.
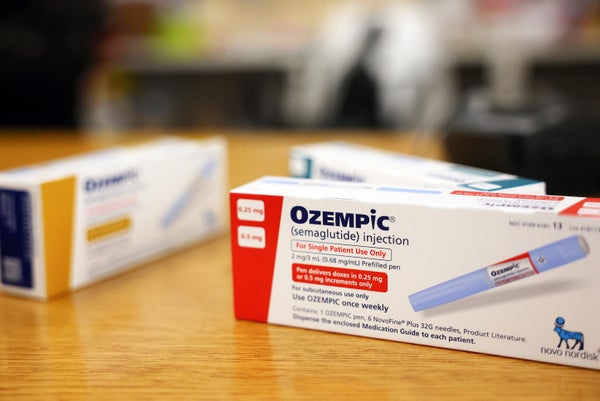
Managing her weight was a losing battle until Morris’ doctor prescribed a Type 2 diabetes medication, Ozempic, four months ago. It’s one in a new category of medications changing how ordinary people as well as medical experts think about obesity, a condition that affects nearly 4 in 10 people 60 and older.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
The drugs include Ozempic’s sister medication, Wegovy, a weight loss drug with identical ingredients, which the FDA approved in 2021, and Mounjaro, approved as a diabetes treatment in 2022. (Ozempic was approved for diabetes in 2017.) Several other drugs are in development.
The medications reduce feelings of hunger, generate a sensation of fullness, and have been shown to help people lose an average of 15% or more of their weight.
“It takes your appetite right away. I wasn’t hungry at all and I lost weight like mad,” said Morris, who has shed 40 pounds.
But how these medications will affect older adults in the long run isn’t well understood. (Patients need to remain on the drugs permanently or risk regaining the weight they’ve lost.)
Will they help prevent cardiovascular disease and other chronic illnesses in obese older adults? Will they reduce rates of disability and improve people’s ability to move and manage daily tasks? Will they enhance people’s lives and alleviate symptoms associated with obesity-related chronic illnesses?
Unfortunately, clinical trials of the medications haven’t included significant numbers of people ages 65 and older, leaving gaps in the available data.
While the drugs appear to be safe — the most common side effects are nausea, diarrhea, vomiting, constipation, and stomach pain — “they’ve only been on the market for a few years and caution is still needed,” said Mitchell Lazar, founding director of the Institute for Diabetes, Obesity and Metabolism at the University of Pennsylvania Perelman School of Medicine.
Given these uncertainties, how are experts approaching the use of the new obesity medications in older people? As might be expected, opinions and practices vary. But several themes emerged in nearly two dozen interviews.
The first was frustration with limited access to the drugs. Because Medicare doesn’t cover weight loss medications and they can cost more than $10,000 a year, seniors’ ability to get the new drugs is restricted.
There is an exception: Medicare will cover Ozempic and Mounjaro if an older adult has diabetes, because the insurance program pays for diabetes therapies.
“We need Medicare to cover these drugs,” said Shauna Matilda Assadzandi, a geriatrician at the University of Pittsburgh who cares for Morris. Recently, she said, she tried to persuade a Medicare Advantage plan representative to authorize Wegovy for a patient with high blood pressure and cholesterol who was gaining weight rapidly.
“I’m just waiting for this patient’s blood sugar to rise to a level where diabetes can be diagnosed. Wouldn’t it make sense to intervene now?” she remembered saying. The representative’s answer: “No. We have to follow the rules.”
Seeking to change that, a bipartisan group of lawmakers has reintroduced the Treat and Reduce Obesity Act, which would require Medicare to cover weight loss drugs. But the proposal, which had been considered previously, has languished amid concerns over enormous potential costs for Medicare.
If all beneficiaries with an obesity diagnosis took brand-name semaglutide drugs (the new class of medications), annual costs would top $13.5 billion, according to a recent analysis in The New England Journal of Medicine. If all older obese adults on Medicare — a significantly larger population — took them, the cost would exceed the total spent on Medicare’s Part D drug program, which was $145 billion in 2019.
Laurie Rich, 63, of Canton, Massachusetts, was caught off guard by Medicare’s policies, which have applied to her since she qualified for Social Security Disability Insurance in December. Before that, Rich took Wegovy and another weight loss medication — both covered by private insurance — and she’d lost nearly 42 pounds. Now, Rich can’t get Wegovy and she’s regained 14 pounds.
“I haven’t changed my eating. The only thing that’s different is that some signal in my brain is telling me I’m hungry all the time,” Rich told me. “I feel horrible.” She knows that if she gains more weight, her care will cost much more.
While acknowledging difficult policy decisions that lie ahead, experts voiced considerable agreement on which older adults should take these drugs.
Generally, the medications are recommended for people with a body mass index over 30 (the World Health Organization’s definition of obesity) and those with a BMI of 27 or above and at least one obesity-related condition, such as diabetes, high blood pressure, or high cholesterol. There are no guidelines for their use in people 65 and older. (BMI is calculated based on a person’s weight and height.)
But those recommendations are problematic because BMI can under- or overestimate older adults’ body fat, the most problematic feature of obesity, noted Rodolfo Galindo, director of the Comprehensive Diabetes Center at the University of Miami Health System.
Dennis Kerrigan, director of weight management at Henry Ford Health in Michigan, a system with five hospitals, suggests physicians also examine waist circumference in older patients because abdominal fat puts them at higher risk than fat carried in the hips or buttocks. (For men, a waist over 40 inches is of concern; for women, 35 is the threshold.)
Fatima Stanford, an obesity medicine scientist at Massachusetts General Hospital, said the new drugs are “best suited for older patients who have clinical evidence of obesity,” such as elevated cholesterol or blood sugar, and people with serious obesity-related conditions such as osteoarthritis or heart disease.
Since going on Mounjaro three months ago, Muriel Branch, 73, of Perryville, Arkansas, has lost 40 pounds and stopped taking three medications as her health has improved. “I feel real good about myself,” she told me.
When adults with obesity lose weight, their risk of dying is reduced by up to 15%, according to Dinesh Edem, Branch’s doctor and the director of the medical weight management program at the University of Arkansas for Medical Sciences.
Still, weight loss alone should not be recommended to older adults, because it entails the loss of muscle mass as well as fat, experts agree. And with aging, the shrinkage of muscle mass that starts earlier in life accelerates, contributing to falls, weakness, the loss of functioning, and the onset of frailty.
Between ages 60 and 70, about 12% of muscle mass falls away, researchers estimate; after 80, it reaches 30%.
To preserve muscle mass, seniors losing weight should be prescribed physical activity — both aerobic exercise and strength training, experts agree.
Also, as older adults taking weight loss drugs eat less, “it’s critically important that their diet includes adequate protein and calcium to preserve bone and muscle mass,” said Anne Newman, director of the Center for Aging and Population Health at the University of Pittsburgh.
Ongoing monitoring of older adults having gastrointestinal side effects is needed to ensure they’re getting enough food and water, said Jamy Ard, co-director of Wake Forest Baptist Health’s Weight Management Center.
Generally, the goal for older adults should be to lose 1 to 2 pounds a week, with attention to diet and exercise accompanying medication management.
“My concern is, once we put patients on these obesity drugs, are we supporting lifestyle changes that will maintain their health? Medication alone won’t be sufficient; we will still need to address behaviors,” said Sukhpreet Singh, system medical director at Henry Ford’s weight management program.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.