Osteosarcoma is the most common form of bone cancer, but it has a poor prognosis, with only 15–20% of patients remaining cancer-free for two years. Currently, the main form of treatment for osteosarcoma is immunotherapy, which involves modifying a patient’s T cells to target antigens expressed on tumour cells. Researchers have found that using chimeric antigen receptor (CAR) T cells targeted to tumour-specific antigens can significantly improve treatment efficacy.
Clinical techniques used to monitor the activity and distribution of CAR T cells in tumours include flow cytometry and analysis of blood samples, or biopsies of sites with CAR T cell activity. Although these existing approaches are useful, flow cytometry measurements from circulating T cells do not accurately represent the response at the tumour site, while repeated invasive biopsies are not practical for patients.
As an alternative method for visualizing the CAR T cell distribution, a research team headed up at Stanford University proposes labelling CAR T cells with nanoparticles, which can then be monitored with several imaging modalities. The researchers investigated the use of ferumoxytol, an approved iron supplement made of iron oxide nanoparticles, which can be detected with magnetic resonance imaging (MRI), photoacoustic imaging and magnetic particle imaging. The researchers believe that monitoring the distribution of ferumoxytol-labelled CAR T cells could help optimize and personalize treatment regimes.
In vivo imaging of nanoparticle-labelled CAR T cells
Lead author Louise Kiru and colleagues, also from Georgia Institute of Technology and the University of Pennsylvania, have developed a clinically-translatable technique to label CAR T cells with ferumoxytol. To evaluate this method, they assessed the viability and functionality of ferumoxytol-labelled CAR T cells, reporting their findings in the Proceedings of the National Academy of Sciences. They also investigated the optimal multimodal imaging technique to monitor the accumulation of the labelled cells in the tumour.
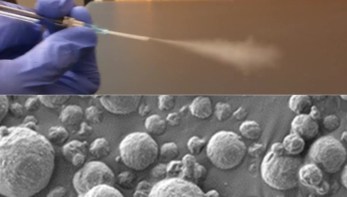
The researchers used a microfluidics device to label the CAR T cells with ferumoxytol via mechanoporation, a technique that involves imparting physical force onto the cell membrane to create nanopores for the delivery of nanoparticles. This approach significantly improved the uptake of iron per cell in comparison with traditional co-incubation techniques. Using bioluminescence imaging, the researchers found that mechanoporation had minimal impact on the viability of ferumoxytol-labelled CAR T cells. They also demonstrated that the function of CAR T cells in vitro was not impacted by the labelling process.
Next, the researchers used T2*-weighted MRI to monitor the accumulation of ferumoxytol-labelled CAR T cells in osteosarcoma-bearing mice, before the infusion of cells and for three consecutive weeks afterwards. They identified iron enhancement in the tumour one week after administration, as a result of nanoparticle labelling. Additionally, they observed that the iron signal in the tumour vasculature slowly dissipated. This indicates that ferumoxytol-labelling can enhance the infiltration of T cells in the tumour whilst diluting the iron level in CAR T cells.
The researchers also identified a correlation between the accumulation of ferumoxytol-labelled CAR T cells at week 1, as determined with MRI, and the decrease in tumour size at week 3. Following an initial increase in tumour size due to pseudo-progression, three weeks after administration of the ferumoxytol-labelled CAR T cells they noted a 13-fold reduction in tumour size compared with pre-treatment images. This indicates that labelling with ferumoxytol does not affect the CAR T cells’ ability to treat tumour cells. “Our data suggest that ferumoxytol MRI could serve as a predictive biomarker for tumour response to CAR T cell therapy,” says Kiru.
Finally, monitoring the accumulation of ferumoxytol-labelled CAR T cells using photoacoustic imaging confirmed the findings from MRI. Similarly, the team utilized magnetic particle imaging for direct quantification of iron oxide nanoparticles and observed a greater concentration of iron in the tumour at week 1 compared with unlabelled-CAR T cells.
The future of CAR T cell imaging
In addition to successful labelling of CAR T cells with iron oxide nanoparticles, Kiru and colleagues have demonstrated the ability to monitor the accumulation of these labelled cells for osteosarcoma treatment, using a variety of imaging techniques. “The imaging approach can be used to monitor the localization of the therapeutic cells in a dose-dependent manner and contribute to elucidating the factors that give rise to responders and non-responders of T cell therapy for solid tumours,” they say.
In future, the researchers envision wider implementation of this technique. “While an osteosarcoma model is used here, it is possible to use this imaging strategy for tracking other therapeutic cells, including CAR T cells targeted to glioblastoma, where strategies for tracking therapeutic cells in the brain are limited,” they write.