Esther Oladejo knew she'd crossed an invisible boundary when she started forgetting to eat for entire days at a time. A gifted rugby player, Oladejo had once thrived on her jam-packed school schedule. But after she entered her teenage years, her teachers started piling on assignments and quizzes to prepare students for high-stakes testing that would help them to qualify for university.
As she devoted hours on hours to cram sessions, Oladejo's resolve began to fray. Every time she got a low grade, her mood tanked—and with it, her resolve to study hard for the next test. “Teachers [were] saying, ‘Oh, you can do much better than this,’” says Oladejo, now 18, who lives in Merseyside, England. “But you're thinking, ‘Can I? I tried my best on that. Can I do any more than what I've done before?’”
One morning, as Oladejo steeled herself for another endless day, her homeroom teacher passed out a questionnaire to the students, explaining that it would help assess their moods and well-being. Oladejo filled it out, her mind ticking forward to her upcoming classes.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Soon after that, someone called to tell her she'd been slotted into a new school course called the Blues Program. Developed by Oregon Research Institute psychologist Paul Rohde and his colleagues at Stanford University, the program—a six-week series of hour-long group sessions—teaches students skills for managing their emotions and stress. The goal is to head off depression in vulnerable teens.
Although Oladejo didn't know it at the time, her course was one in an expanding series of depression prevention programs for young people, including Vanderbilt University's Teens Achieving Mastery Over Stress (TEAMS); the University of Pennsylvania's Penn Resiliency Program; Happy Lessons, developed by Dutch social scientists; and Spain's Smile Program. The growing global interest in depression prevention is helping to establish the efficacy of a range of programs in diverse settings.
For researchers heading up depression prevention programs, the stakes of early intervention couldn't be higher. The earlier a first episode of depression begins, and the more episodes a person suffers, the more serious and disabling the condition is likely to be throughout life. People who recover from an initial depression have a 40 to 60 percent chance of a later episode; those with two episodes have a 60 to 70 percent chance of recurrence, and those with three episodes have a 90 percent chance—a vicious cycle that too often ends in chronic illness or disability. And since the COVID pandemic, teens' risk of falling into the cycle has climbed: 42 percent of U.S. high school students report lasting sadness or hopelessness in surveys by the Centers for Disease Control and Prevention, up from 28 percent a decade before.
Prevention courses like the one Oladejo took offer hope to halt this trend. Intervention during the teen years, studies suggest, can potentially stop the kind of depressive cascade that erodes human potential and imposes massive costs on health-care systems. “It's a chronic episodic illness, and relapse is very common,” says Brown University psychologist Tracy Gladstone. “If you can avoid that initial episode, I think you're really setting people on a much better path.”
Courses for at-risk young people have forestalled depression, numerous studies have found, reducing rates of onset by up to half in the months and years following the programs. Yet program developers have struggled to make a convincing case for prevention amid unprecedented levels of need for acute care during an ongoing global mental health crisis.
Feeling like she didn't have much to lose, Oladejo agreed to give the Blues Program a try. The message she was getting from teachers “was like, ‘You've got to get ready, we've got to do this.’ I was 15—I don't really know what I want to do in my life quite yet,” she says. “I was starting to spiral.”
Health experts and political leaders have been brainstorming ways to ward off mental illnesses such as depression, bipolar disorder and schizophrenia for decades. In a 1963 speech to Congress, President John F. Kennedy described plans for a comprehensive preventive approach at the federal level. The initiative would include “selected specific programs directed especially at known causes” of mental illnesses, Kennedy proposed, but would also involve “the general strengthening of our fundamental community, social welfare, and educational programs.”
Such plans stalled during economic crises in the 1970s. Under President Ronald Reagan, federal spending on social programs decreased, and national mental illness prevention mostly receded into the background.
But rising rates of mental illness through the 1990s, especially in young people, helped to rekindle broader interest in prevention. In a 1994 report called “Reducing Risks for Mental Disorders,” the Institute of Medicine (now the National Academy of Medicine) argued for assessing people's mental health vulnerabilities early in life to stave off the worst outcomes.
By the late 1990s and early 2000s researchers were testing several prevention programs for depression, one of the most common mental disorders. Many of these programs were rooted in the cognitive-behavioral practice of correcting harmful thinking patterns—an approach that has consistently reduced depressive symptoms in studies. Among the first prevention offerings were the Penn Resiliency Program, a series of 12 group classes lasting 90 minutes each, and the Australia-based Resourceful Adolescent Program, consisting of 11 group sessions of 50 minutes.
Around this time Rohde was a young psychologist at the Oregon Research Institute (ORI), a small company with National Institutes of Health funding. Early in his career, Rohde had helped develop Adolescent Coping with Depression, one of the first standardized group treatments for depressed teens.
When psychologist Eric Stice joined Rohde's research group in the mid-2000s, Rohde and his colleagues started focusing on depression prevention. Stice specialized in preventing eating disorders, and his graduate student Sarah Kate Bearman wanted to see how much a similar approach could help teens on the cusp of depression. Bearman's graduate thesis described an early iteration of the Blues Program, teaching teens cognitive-behavioral skills in four one-hour sessions. Rohde liked the way this program component condensed cognitive principles into digestible lessons—and he liked that it took less time than competitors such as the Penn Resiliency Program, which could make it easier for schools and agencies to implement.
After Bearman graduated, Rohde, Stice and Stanford researcher Heather Shaw continued to develop the Blues Program and test it at a number of pilot sites. Having watched depression disrupt his clients' lives year after year, Rohde was fired up about the idea of bending teens' mental health curve for a lifetime. “We know that if we can prevent depression in young adulthood, we're going to prevent recurrent episodes of depression,” he says. “We're going to reduce future suffering.”
It makes intuitive sense that preventing a first depressive episode could reshape someone's mental health trajectory. Less intuitive, and less well known, are the biological stakes involved in keeping depression at bay. During each bout of depression, brain tissue can shrink—especially in the hippocampus and prefrontal cortex, which govern memory, emotion and higher-order thinking. It's unclear whether this brain atrophy can be fully reversed. The decrease in tissue is also linked to future bouts of depression. In recovered people who relapsed, the brain's cortical volume shrank over a two-year period, whereas recovered people who did not relapse showed no such change.
Brain changes during adolescence may make teens especially vulnerable to depression and the cellular havoc it wreaks. In a study from McLean Hospital in Belmont, Mass., young people who experienced hardship such as emotional abuse at age 14 or 15 were more likely to become depressed compared with those who faced such adversity earlier or later in life. Prolonged stress, research shows, may be more damaging to the brain during this time—and another study suggests that early stress-linked brain changes may make people more vulnerable to depression.
Rates of depression steadily climb during the teen years, so some specialists contend that the earlier teens enroll in prevention programs, the better. “The adage that an ounce of prevention is worth a pound of cure is really true in this setting,” says adolescent psychiatrist Elizabeth Ortiz-Schwartz of Silver Hill Hospital in Connecticut. “We need to start looking at early adolescence.” Rohde concurs, which is why he, Stice and Shaw designed the Blues Program to serve students as young as 12. The first step in Blues—now offered at sites in Pennsylvania, Texas and Utah, as well as in the U.K.—is screening school populations for high-risk students like Oladejo. These students report sleep problems, low self-esteem or low interest in daily activities, but their symptoms aren't severe enough for a depression diagnosis. (Some symptoms rule teens out of the program; if they report feeling suicidal, they're referred to acute treatment.) Gauging students' distress from the questionnaire works better than probing into their family histories. “For us, it's easiest just to ask the student if they have some symptoms,” Rohde says, adding that when teens are struggling, “that provides motivation for working on skills.”
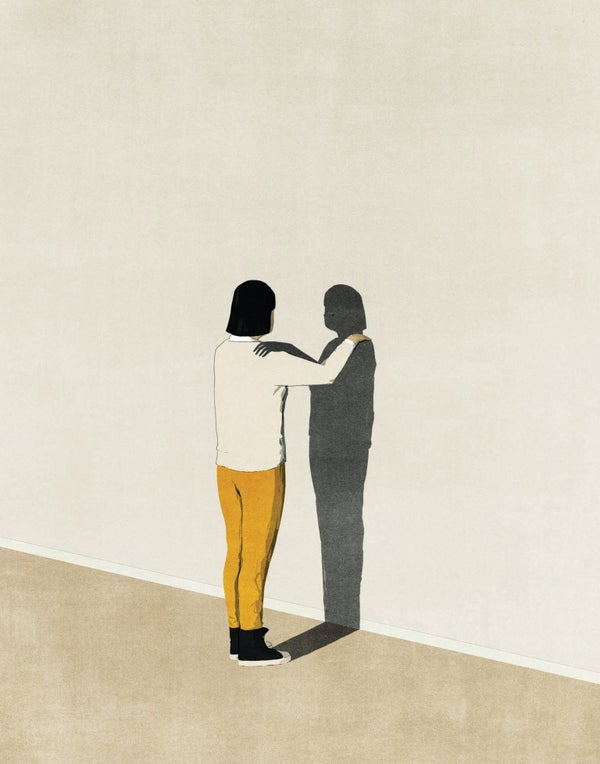
From there, facilitators organize qualifying students into small groups and teach them cognitive tactics they can use to process difficult events. Many of these measures resemble those therapists teach depressed clients, but the Blues Program introduces them as a kind of vaccination strategy. When teens learn how to keep stress in check, the theory goes, they'll be able to defuse new stressors before their emotional impact explodes.
One teaching tool in the program is the “triangle of feelings, thoughts and actions,” which illustrates that the way people think about what happens influences how they feel overall—and, by extension, how motivated they are to take helpful action. A negative thought—such as “No one loves me” after a romantic rejection—can make you feel miserable, and when you feel miserable, you'll be less likely to risk asking someone else out. Thinking of the rejection as a painful episode that you can get through, in contrast, can stop the cycle of misery.
The triangle concept clicked for Esther Oladejo. “It basically made you think, Do I want this small situation to dictate how the rest of my life's going to go?” Oladejo says. She could see how her own reactions followed the pattern: after she flubbed an assignment, she'd beat herself up and feel worthless, and that sense of worthlessness made it hard to tackle the next round of papers and tests.
In later sessions of Blues, facilitators explain how to challenge negative thoughts—for example, by brainstorming a new thought that's less exaggerated and more optimistic than the original. “Is there another way to think about this situation?” session leaders ask. “What advice would you give a friend who was feeling the way you do?”
After that, students share their new thoughts with the rest of the group. For Oladejo, an initial gut reaction—“I tanked that test. I suck at school”—might morph into “This isn't my final exam. I can learn from this and do better on the end-of-year test.” It isn't the precise content of the revamped thought that matters. “There is not a single right counterthought to a given negative thought,” group leaders tell students. “Figure out whether a particular new thought makes sense to you.”
The Salt Lake County Department of Youth Services (DYS) occupies a cluster of squat tan buildings ringed by distant snow-topped mountains. Dozens of students congregate there every semester, virtually and in person, developing new cognitive skills designed to help them evade depression. A blue “Heroes Work Here!” banner hangs in the front lobby, where I meet Jodi Rushton, the effervescent social worker who heads up Salt Lake's version of the Blues Program. She leads me into a bright classroom, the table stacked with sandwiches and chip bags for the teens who'll drop in this afternoon.
Rushton tells me that the DYS serves a population at risk for mood disorders—about one in three Utah teens report depressive symptoms—and the Blues Program seemed like a natural fit when she saw it on a list of evidence-based options several years ago. “We were teaching pretty outdated programs,” Rushton says. “We needed a revamping.”
Enrollment in the program, which DYS staff have renamed “Me Time,” has climbed since its inception, and hundreds of local teens have so far completed the course. After COVID hit in 2020, Rushton and her colleagues scrambled to transfer the program online. They worried Me Time wouldn't translate well into virtual space, but their worries were unfounded. In fact, the opposite was true: As soon as DYS started offering online sessions, enrollment exploded. “It just took off. Transportation, space, time—all these obstacles were eliminated,” Rushton says. “Even after I close registration, I still just get referrals continuously.” She has let teens from other states sign up for Me Time because most have no similar option available locally.
Rushton has a cardinal rule when she leads a session, whether online or in person: Make sure each student gets at least one chance to hold the floor. “It's really interactive,” she says. “A lot of the effectiveness falls on how much attention you can give to everybody—drawing out the teens who maybe are more shy, handling the ones who want to talk all the time.”

Credit: Jen Christiansen; Sources: “Age at Onset of Mental Disorders Worldwide: Large-Scale Meta-analysis of 192 Epidemiological Studies,” by Marco Solmi et al., in Molecular Psychiatry, Vol. 27; June 2, 2021; “Global Prevalence and Burden of Depressive and Anxiety Disorders in 204 Countries and Territories in 2020 Due to the COVID-19 Pandemic,” by Damian Santomauro et al., in Lancet, Vol. 398; October 8, 2021 (data)
After chatting with Rushton, I meet a few local Me Time participants ranging in age from 12 to 17. To protect student privacy, the program is closed to outside observers, but the students told me about the dynamic it fosters. “Everyone knows, like, ‘Think really deeply about if a problem’s as big as you think it is,'” says Monica, the oldest of the group. But the program sessions, she continues, helped her transition from knowing what she should do to actually doing it. “It was really helpful to be able to discuss personal experiences and how we could have changed the way we were thinking,” she says. “Being able to have a group discussion allowed it to stick more. I've kind of taken it to self-reflect every day: ‘Is my reaction fitting the size of this issue?’”
Teens could also learn cognitive-behavioral skills one-on-one with a therapist. But in general, individual therapy can impose a high cost burden on families—and some Salt Lake teens say they like Me Time better than traditional therapy, which tends to have an uneven power dynamic between therapist and client. Me Time “just helps more,” one participant tells me. “You're not put on the spot, and you're able to form a connection with other people.” The give-and-take spirit of Me Time chats helped another student feel less isolated in their mental health struggles. “You could hear other people's situations—how they coped with it or what they did to solve the problem. If it was just one-on-one, I don't think I would have been helped as much.”
Having watched countless Blues Program sessions in action, Rohde agrees. There's something alchemical, he thinks, about teaching cognitive skills in a small-group context. “Part of the value is getting kids together,” he says. “As they feel comfortable, they can share the thoughts and feelings and actions that they're struggling with. That can be helpful for the other students because it normalizes that these kinds of problems are really, really common.”
Like her counterparts in Salt Lake City, Esther Oladejo drew more than she'd expected on the well of support from her small group. She didn't know most of the other students in her Blues class well at first, but their shared trust grew. When other group members shared school or family problems, she advised them as best she could—and felt gratified when they came back to report that her suggestions had helped. In return, they buoyed her in the same way. “I feel like that's really important—someone who's looking at you as if they actually see you,” she says.
School systems in Utah, the U.K., and elsewhere have adopted the Blues Program in part because of the evidence for its effectiveness, Rohde says. After the ORI team secured funding from the National Institutes of Mental Health, they launched a large-scale 2015 Blues Program trial that enrolled 378 Oregon students at risk of depression. Just 10 percent of students who finished the Blues Program had developed depression by the two-year follow-up mark, compared with 25 percent of control group members who read a cognitive-behavioral self-help book called Feeling Good.
A 2018 meta-analysis of four separate Blues Program trials showed that enrolled students were substantially less likely than control subjects to develop depression within two years. Other prevention programs for students at risk, including the Penn Resiliency Program, have also significantly reduced students' depressive symptoms, as have offerings such as Op Volle Kracht (At Full Force) in the Netherlands and Spain's Smile Program.
Salt Lake City's Blues Program site results have largely mirrored these broader ones. During the 2021–2022 school year, students scored notably lower on a standard depression symptom scale after finishing the program, and their scores remained almost as low three months later. And Me Time's new online format seems to work as well as the traditional one: after the program, online participants' depressive symptom scores actually dropped more than those of in-person students. Still, how long these benefits will last remains unknown because studies have not yet been done to assess how many depressive episodes any of these programs might prevent over a lifetime.
The programs that don't hold up as well in trials, at least so far, are those designed to prevent depression in entire school populations. A meta-analysis of more than 40 studies found that schoolwide prevention programs were significantly less effective at staving off depressive symptoms than targeted programs for at-risk young people. Schoolwide programs, Brown University's Gladstone notes, enroll more students who don't have symptoms—and who may therefore be less motivated to master the skills taught in depression prevention programs. “One of the things about these interventions is that they take work,” she says. “It's hard to engage in something when it doesn't have any resonance for you.”
Further trials are underway to determine which program components are most crucial for effective prevention. Along with her colleague Benjamin Van Voorhees, Gladstone has launched a controlled trial comparing two different online depression prevention programs for at-risk students: Teens Achieving Mastery Over Stress (TEAMS) and a self-guided course called CATCH-IT. The study—which has enrolled more than 500 teens from western Illinois, Chicago and Louisville, Ky.—will track not just their depressive symptoms after the programs but how they deal with stress and low moods. So far Gladstone hasn't had any trouble recruiting trial subjects. “It's really difficult to find mental health support,” she says. “Families are just excited about the trial. They want their kids in.”
Despite bursts of local enthusiasm for prevention programs, few school districts or agencies, whether in the U.S. or abroad, have programs like TEAMS or Blues available for struggling teens, and most people are not even aware that such programs exist.
The hard part of broadening the programs' reach, as Gladstone and Rohde have found, isn't convincing teens or families to give them a try. It's convincing those in power that the programs are practical and affordable for resource-strapped communities—and that prevention is worth investing in. Aside from a small one-time fee, schools and nonprofits don't need to pay licensing fees for Blues Program material. But ORI charges organizations $2,800 to train their staff on how to deliver the Blues content to teens, and each local facilitator who wants to instruct other staff must pay thousands more to get certified as a “trainer of trainers.” Administering the program adds to the workloads of counselors, social workers, and other staff, which can oblige managers to pay for more staffing hours or hire more employees.
In general, Gladstone says, depression prevention programs are easiest to implement in countries with national health insurance systems, such as the U.K. These systems, figuring the programs will eventually lead to lower costs for mental health care, are more apt to fund local agencies or nonprofits that offer the programs.
In the U.S., however, “insurance is generally attached to people's jobs, and people switch their jobs,” Gladstone says. “Often there's not really an incentive for insurance companies to fund prevention programs, because by the time somebody would develop the [condition] you're trying to prevent, somebody else will be paying for the treatment.” Although some U.S. insurance companies have started funding exercise programs that prevent physical illness, they don't reliably reimburse providers or agencies for depression prevention programs.
That typically leaves local governments, school districts and nonprofits on the hook to fund prevention efforts. Me Time is in a fortunate position, drawing from the DYS's annual mental health prevention budget of more than $570,000. Across the region, Rushton is trying to increase access to program resources by devoting more time to “training trainers”—briefing school staff members across the Salt Lake region so they can deliver the course to their own students. But this can be a challenging process, she says. “Social workers and counselors, people in schools, are really weighed down. And so even asking them, ‘Hey, we want you to teach this six-week class’—it's kind of a big ask.”
To help make the Blues Program more feasible on a local level, Rohde wants to do more real-world data collection on the practical side of depression prevention programs—how much they'll cost per student, for instance, and how that compares with the cost of treating an already depressed teen. Those kinds of concrete numbers could help convince local decision makers to support the program and health insurance companies to reimburse for it, he says. “It gives them the kind of data they need to say, ‘We're going to prevent this much future treatment cost down the road.’”
But Janet Welsh, principal investigator for Penn State University's Evidence-Based Prevention and Intervention Support program, points out that cost-savings numbers wouldn't necessarily drive wider adoption for depression prevention programs. “To be perfectly honest, I have those data for substance abuse,” says Welsh, who regularly evaluates research-based mental health programs. “I can show you how much it saves to do universal prevention. Yet people still won't do it.”
That reluctance, Welsh says, stems from a basic feature of human psychology: the tendency to value in-the-moment problem solving over avoiding future crises. “Prevention of anything—violence, drug abuse, mental health problems—is always going to be [the less favored option],” she says. If a depressed teen goes to therapy and gets well, her providers can document a clear trend of recovery. But if a student takes a depression prevention course and remains well, it's a different, lowercase kind of triumph, one that can be hard for funders to appreciate when their communities are in mental health crisis. “I can point to some really well-adjusted kids and say, ‘Look, they don't have substance abuse or mental health problems,’” Welsh says. “And you're like, ‘Yeah? So?’”
Despite the challenges of making the case for prevention, Rohde, Gladstone, and others hope that more communities will buy into it—especially given the strong enrollment Blues Program sites have seen since the COVID pandemic began. Clinicians also see opportunities for further honing the programs to attract newcomers, taking steps such as tailoring curricula for students from different backgrounds. A program that works well in California's Bay Area won't necessarily land in urban Detroit, rural England or Alaska Native communities. “Investing in the research and application of those programs is going to be essential,” Ortiz-Schwartz says, “so that districts can find solutions that are more on target with their population.”
Although more data and customized lesson plans may help make the case, those in charge of funding may ultimately look to the human element: how students like Esther Oladejo fare as they approach adulthood. Although Oladejo's mood still drifts up and down at times, she says disputing negative thoughts about her own abilities has given her courage to speak up more and take chances. “Before I probably would have hid away,” she says. “But the structure of being able to think, ‘Okay, what are the benefits? Am I going to be okay doing it?’ Yeah. Let's go.”
That willingness to advocate for herself led Oladejo to an unexpected breakthrough. After finishing the Blues Program and enrolling in college, she continued to flounder academically, and she grew more aware of the mismatch between the hours she put in and the results she was getting. If what you're doing isn't working, Blues lessons had prompted, what are some other ways of solving the problem? She decided to approach a tutor on her college campus to explain her dilemma, and the tutor referred her to the campus support team. After some tests, they told her she had dyslexia, which helped her get proper assistance—and finally make sense of why school had been such a struggle. (It's common for those at risk of depression, like Oladejo, to have other conditions like dyslexia, ADHD or anxiety; the U.S. Preventive Services Task Force has called for kids and teens to be screened for both depression and anxiety so they can get fast, effective treatment.) “I'd put myself down, thinking, ‘Why can't I just get it the first time around?’” Oladejo says of her academic troubles. “But because I was able to use the skills, not be so anxious to ask for help, I was able to get a diagnosis.”
This progression reveals how the decisions people make in one moment, like Oladejo's choice to speak up and get evaluated for learning challenges, lead to a different array of options than those they'd have if they hadn't made that fateful decision. In that sense, it isn't just cognitive skills or stress regulation or a support group atmosphere that counts for teens at risk of depression. It's the way those things equip them to make choices that alter the decision tree itself. For adults who first slid into depression in middle or high school, it's an absorbing thought experiment: If I'd known how to approach that setback differently, how would my choices have been different? And what other choices would have opened up? And then, and then?
It's in the unfolding of these sequences that the promise of prevention is clearest. To help initiate such sequences for others, Oladejo has volunteered with the U.K.-based nonprofit Action for Children, speaking with local officials and lawmakers about her Blues Program experience. She might pursue a psychology doctorate so she can become a therapist—and she has a clear vision of the work she wants to do, helping clients build the kind of group support structure that got her through her own worst days. “I don't want to be like the usual therapist. If I do face-to-face, I want it to be an inclusive session,” she says. “I want to be able to give people that sense they're not alone.”